Overview #
Definitions
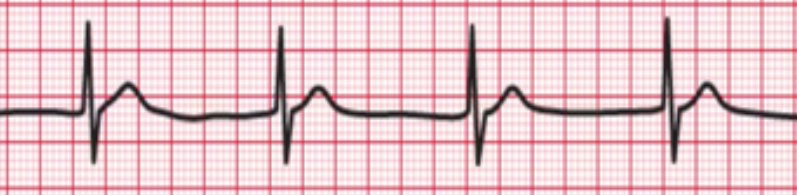
- Bradycardia refers to a heart rate less than 60 beats per minute in an adult
Prioritization
- Urgent if hemodynamically unstable or symptomatic (chest pain, altered mental status, shortness of breath, hypotension)
Key points
- Determine if the patient is hemodynamically unstable or stable
- Determine if the bradycardia is symptomatic or asymptomatic
- Determine the anatomic location causing the bradycardia – a narrow QRS is likely to indicate a problem above the bundle of HIS and is likely able to be managed with medications while a wide QRS indicates a problem in the bundle of HIS which requires pacing more often than not
- Assess for and remove reversible causes of the bradycardia
- Progressive bradycardia or worsening bradycardia of seconds-minutes is a peri-arrest sign
Triage #
Hemodynamically unstable and symptomatic (hypotension, agitation, association with acute MI) → emergency requiring immediate attention
Hemodynamically stable and non symptomatic → non urgent review
Causes #
Sinus bradycardia(1)
Junctional bradycardia
First degree AV block
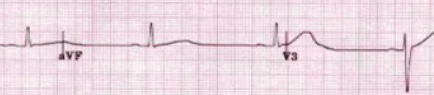
Second degree AV block – Type 1

Second degree AV block – Type 2

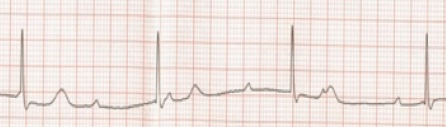
Third degree (complete AV block)
AF with slow ventricular rate
Drugs: antiarrhythmic agents such as beta-blockers, calcium channel blockers, digoxin, amiodarone, sotalol
Cardiac disease: acute MI, sick sinus syndrome, myocarditis etc, post cardiac surgery
Other: health young athletes, vasovagal, electrolyte disturbances, hypothermia, hypothyroidism, sick sinus syndrome, obstructive sleep apnea, raised ICP, central nervous system conditions: stroke, trauma to cervical or thoracic spine, infection
Clinical features #
History
● Characterize heart rate
● Recent ischaemic symptoms: chest pain, SOB, nausea or vomiting or signs of end organ dysfunction such as altered mental state, syncope
● Any medications/drugs eg. digoxin, a beta blocker, calcium channel blocker or anti-arrhythmic drug
● History of cardiac risk factors: smoking, hypertension, hypercholesterolemia, diabetes, renal impairment or family history, history of angina/previous acute myocardial infarction
Examination
● Vital signs
○ Hypothermia
○ Hypothyroidism
○ Hypertension
○ Altered mental state
Peripheries – cool extremities suggesting poor end organ perfusion
● Abdomen
○ Palpable kidney mass
● Cardiovascular
○ Mitral regurgitant murmur (recent acute MI)
- Respiratory
○ Signs of respiratory distress and pulmonary oedema
● GIT
○ Renal, aortic or femoral bruits (atherosclerosis)
Urine output
- Reduced suggest sign of reduced end organ perfusion
Investigations #
| Investigation | Indication |
| ECG | Observe rhythm, determining the anatomic location of the bradycardia (narrow – AV/SA node disease; wide – proximal or distal disease) |
| Troponin | If concerned about potential myocardial ischemia |
| FBE | Anaemia leading to MI, WBC for infective cause (eg, lyme disease, endocarditis) |
| UEC | Electrolyte disturbance, renal disease potentially precipitated electrolyte disturbance |
| TFT | Hypo/hyperthryoidism |
| Digoxin Level | To assess digoxin toxicity/overdose |
Further Investigations #
| Investigation | Indication |
| Holter monitor | If bradyarrhythmia is suspected but cannot be captured on normal ECG |
| Transthoracic echocardiogram | Structure and functional of the heart (eg. previous MI leading to arrthymia) |
Management – hemodynamically unstable (2) #
Please see guideline 11.9 – Managing Acute Dysrhythmias from the Australia Resuscitation Council for reference – https://resus.org.au/guidelines/ (2)
In patients with signs of circulatory compromise (chest pain, SOB, hypotension or altered mental status) or if heart rate is less than 40 beats/min
- Resuscitation (3)
- Obtain IV access
- Monitor ECG, BP, oxygen saturations (provide supplemental if needed)
- Get senior help involved early
- Administer IV atropine (4)
| Atropine 0.5 mg intravenously, repeat after 3 to 5 minutes if necessary, up to a maximum of 3 mg. |
- Should this be unsuccessful, consider adrenaline, isoprenaline and transcutaneous pacing as temporising measures follow by transvenous pacing (3, 4, 5)
| Isoprenaline 2 to 10 micrograms/minute by intravenous infusion, titrated according to clinical responseOR Adrenaline 2 to 10 micrograms/minute by intravenous infusion, titrated according to clinical response |
- Treat reversible courses (eg. calcium/insulin for potassium, thyroxine for myxeoedema coma, warming for hypothermia, antibiotics for infection)
- Consult cardiology
- Consideration of permanent pacemaker (5)
- Consider ICU transfer
In the case of bradycardia due to AV block complicating acute myocardial infarction, reperfusion therapy in the form of urgent percutaneous coronary intervention if available or fibrinolysis is desirable (4)
Management – haemodynamically stable #
Sinus and AV nodal dysfunction (narrow QRS) rarely leads to life-threatening complications and are treated with watchful waiting, atropine or sympathetic medications such as adrenaline. Distal His-Purkinje block (wide QRS) is much more serious, and tend not to respond to atropine and sympathetic stimulation. These patients almost always need pacing and a definitive pacemaker(2).
Sinus bradycardia
- Reassure patient
Junctional bradycardia
- Occurs when electricity activity at the SA node is blocked or less than the automaticity of the AV node/HIS bundle. The rate is usually <40bpm with a narrow QRS, p waves retrograde, narrow or absent
- Can also be preceded in the context of post cardiac valve surgery and inferior MI with RV extension or posterior MI
- Withhold medications such as beta blockers, calcium channel blocks, digoxin poisoning
Atrial fibrillation with slow ventricular response
- Does not require treatment unless there are signs of haemodynamic instability or organ hypoperfusion
- Definitive treatment includes discontinuing drugs that depress cardiac conduction or insertion of permanent pacemaker placement
Atrioventricular block
- First degree
- Usually asymptomatic and is benign
- Second degree
- Mobitz type 1 – ongoing monitoring in setting of ACS or drug toxicity, may progress to complete heart block
- Mobitz type 2 – Commonly progresses to complete heart block
- Third degree
- NOTE: The presence of a new slow bundle branch block against a sinus tachycardia is concerning for complete AV block requiring pacing.
Management of second degree Mobitz type 2- and third-degree AV block (especially symptomatic patients) (5)
- Liaise with cardiology
- Continuous ECG monitoring
- Consideration for further imaging such as a transthoracic echocardiogram
- Cease contributory medications
- Consideration of transvenous pacing
- Consideration for ICU
- Consideration of permanent pacemaker if no reversible causes are identified
References #
- Homoud M. Sinus bradycardia. In: Glassock R, Lam A, editors. UpToDate. [Internet]. Waltham (MA): UpToDate Inc; 2021. [updated 16 Febryary 2021; cited 5 November 2021]. Available from: https://www.uptodate.com/contents/sinus-bradycardia?search=bradycardia&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- The ARC Guidelines [Internet]. Melbourne (Vic): Australian Resuscitation Council; 2021.; [updated 2009 Mar; cited 2021 Nov 8]. Available from: https://resus.org.au/guidelines/
- Neumar RW, Otto CW, Link MS, et al. Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122 (18_suppl_3): p.S729-S767. doi: 10.1161/circulationaha.110.970988
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay. J Am Coll Cardiol. 2019; 74 (7): p.e51-e156. doi: 10.1016/j.jacc.2018.10.044
- eTG complete [Internet]. Melbourne (Vic): Therapeutic Guidelines Ltd; 2018.; [updated 2021 Mar; cited 2021 Nov 8]. Available from: https://tgldcdp.tg.org.au/viewTopic?topicfile=bradyarrhythmias&guidelineName=Cardiovascular&topicNavigation=navigateTopic#toc_d1e98833
Contributors
Reviewing Consultant/Senior Registrar
Dr George He
Dr Joshua Wong